Focus on Sleep Health: On Bruxism at Night (1)
Night teeth grinding is so common in life that people may often "think nothing of it," but in fact, long-term teeth grinding can have adverse effects on health. The related research and treatment of night molars are constantly updated and developed, and the relevant situation is described below.

I.Definition of night molar
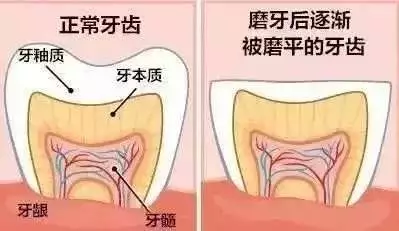
It is important to understand that sleep bruxism (SB) belongs to one type of bruxism, the other is clenching, that is, the involuntary clenching of the teeth during the day, but no sliding friction between the upper and lower teeth, and the mixed type that exists during the day and night. Some studies talk about bruxism, often referring to night bruxism, which actually Narrows it down. At present, there is no exact unified definition of night bruxism, which is mainly distinguished in the two fields of sleep medicine and stomatology. The International Classification of Sleep Disorders points out that night teeth grinding is usually related to sleep awakening, and is the oral activity of teeth grinding or clenching during sleep, which is a sleep-related movement disorder. In prosthodontics, it is believed that an unconscious oral habit, rhythmic, spasmodic non-functional clenching, grinding and making sounds, which is not a functional action of chewing, can lead to occlusal damage and is a risk factor for a variety of oral diseases. In order to be applicable to clinical practice, some scholars have a comprehensive definition: in the unconscious state of sleep, when the teeth are subjected to a certain intensity of bite force, the mandible does rhythmic or large displacement movement, and the anatomical structure of the temporomandibular joint, teeth and other non-physiological actions.
2. Epidemiological investigation and diagnosis of night molars
There are few researches on the current situation of night bruxism in China. A study of 817 samples in Hebei showed that the adult prevalence was 14.4%. Due to the different ways of judging night bruxism, a number of foreign studies reported that the prevalence of night bruxism was between 5.5% and 31.6%, with an average of 12.8%, and the prevalence showed a decreasing trend with the increase of age.
Usually, night bruxism can be diagnosed through patient reports and physician visits, clinical examinations, oral molds, or recording of muscle activity. The questionnaire survey and self-report methods have the limitations of forgetting data or not conforming to the actual situation. Polysomnography is now considered to be the most accurate way to diagnose night bruxism. This system includes electroencephalogram, electroophthalmogram and electromyography of suprhyoid muscle, anterior jugular muscle, masseter muscle and temporal muscle, and can identify signs of bruxism during sleep. Relevant criteria are:Molar attacks ≥2 times/hour, or more than 30 times/night; (2) During each molar attack, the EMG burst more than 6 times, or ≥25 times/hour; ③ At least two grinding sounds were recorded during the night.
Three, the cause of night molar
There is no single cause for night grinding, and the cause is not fully understood, but there is evidence that the following factors are involved.
3.1 Mental and psychological aspects: With the development of the understanding of the bio-psycho-social medical model, it is found that the disease is closely related to mental stress, anxiety and depression. The higher the degree of depression, the more frequently it occurs.

3.2 Occlusal and maxillofacial joints: The main factor is the disharmony of occlusal relationship. During the period of children's dental exchange, the teeth cannot be occluded well, and the subconscious grinding of teeth makes the upper and lower teeth more in contact, which may be the reason for the high prevalence rate in children. Most people think temporomandibular joint disorder is closely related to night molars.
3.3 Sleep disorders: insomnia patients are prone to anxiety and depression, mental pressure can cause night teeth grinding. Sleep apnea patients often snore, tongue fall, airway lumen shrink, may trigger the self-protection mechanism of stress, unconsciously slide the mandible, adjust the oropharyngeal ventilation space. Teeth grinding may also be associated with central microarousal due to hypoxia in apnea. A foreign study recorded that most teeth grinding occurred at the end of apnea events. The number of teeth grinding was proportional to the severity of sleep apnea.
3.4 Neuroendocrine aspects: Studies have reported that the urinary catecholamine level of patients with night molar is higher than that of the normal population. Due to changes in the amount of various endocrine hormones, such as dopamine, norepinephrine, etc., it may disturb the basal ganglia feedback balance and make the coordinated movement of masticatory muscle abnormal.
3.5 Life habits: night grinding often occurs in the lateral or prone position. Due to the lateral pressure on the jaw, the teeth are in a non-median contact state, and the mandibular deviation causes the temporomandibular joint and its surrounding muscle tissue to tense, thus increasing the possibility of night grinding. They exhibit involuntary muscle tremor movements that eventually lead to non-functional tooth wear. Long-term unilateral chewing may be a risk factor for the occurrence of night bruxism. In addition, other factors such as smoking, alcoholism, intake of large amounts of coffee, and abuse of psychotropic drugs may cause night grinding.
3.6 Genetic aspects: Most scholars believe that night grinding is caused by genetic heterogeneity, not a single gene. Specific genes were found to be associated with the onset of night bruxism, and there may be genetic predisposition.
reference
1. Ma Chi, Lu Xiao 爔, et al. Analysis of night bruxism and its related factors in a college student in Hebei Province [J]. Journal of Modern Stomatology, 2019,35(03):181-184. (in Chinese)
2. Yang Rui-mei. Occlusal and sleep characteristics of patients with night bruxism and the therapeutic effect of elastic occlusal pads [J]. World Journal of Sleep Medicine, 21,8(02):216-217.
3.Goldstein G, DeSantis L, Goodacre C. Bruxism: Best Evidence Consensus Statement. J Prosthodont. 2021 Apr; 30(S1):91-101.
4.Kuang B,Li D,Lobbezoo F, et al. Associations between sleep bruxism and other sleep-related disorders in adults: a systematic review. Sleep Med. 2022; 89-31-47.
5.Kale SS, Kakodkar P, Shetiya SH. Assessment of oral findings of dental patients who screen high and no risk for obstructive sleep apnea (OSA) reporting to a dental college - A cross sectional study. Sleep Sci. 2018 Mar-Apr; 11 (2) : 112-117.
6.Polmann H, Reus JC,Massignan C, et al. Association between sleep bruxism and stress symptoms in adults: A systematic review and meta-analysis. J Oral Rehabil. 2021; 48 (5):621-631.
7.Yalcin Yeler D, Yilmaz N, Koraltan M, et al. A survey on thepotential relationships between TMD, possible sleep bruxism, unilateral chewing, and occlusal factors in Turkish universitystudents. Cranio, 2017,35 (5) : 308-314.
8.Campello CP,Moraes SLD,Vasconcelos BCDE, et al. Polymorphisms of the serotonin receptors genes in patients with bruxism: a systematic review. J Appl Oral Sci. 2022; 29:e20210262.
Author:
Liu Lin, Deputy Chief physician, Associate professor
Standing Committee and Director General of Sleep Medicine Branch of Chinese Geriatric Society
Dr. Libo Zhao

